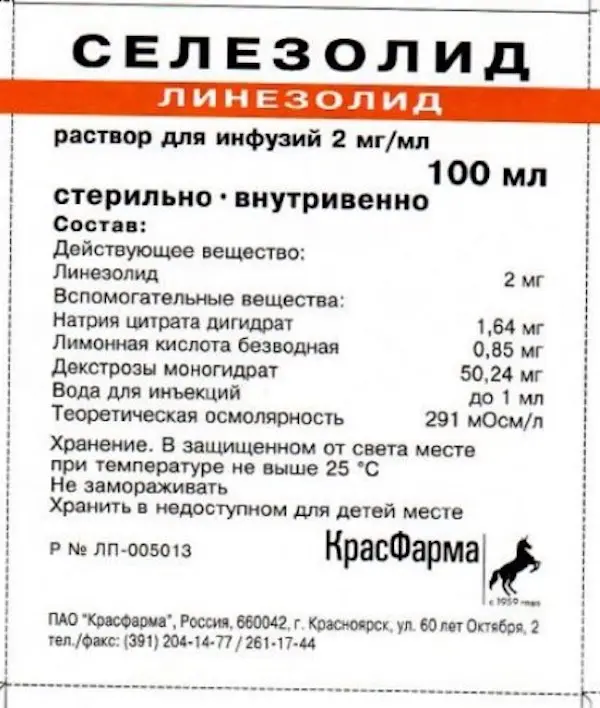
Description
Selezolid Pharmacodynamics
Synthetic antibacterial agent of oxazolidinone group.
Mechanism of action is due to selective inhibition of protein synthesis in bacteria. Due to binding to 23S and 50S subunits of bacterial ribosome, it prevents formation of functional initiating complex 708 of ribosome, which is a component of translation process during protein synthesis.
The drug is active in vitro and in vivo against the following microorganisms:
Gram-positive aerobes: Enterococcus faecium (including vancomycin-resistant strains), Staphylococcus aureus (including methicillin-resistant strains), Streptococcus agalactiae, Streptococcus pneumoniae (including polyresistant strains), Streptococcus pyogenes.
The drug is active in vitro against the following microorganisms:
Gram-positive aerobes: Enterococcus faecalis (including vancomycin-resistant strains), Enterococcus faecium (vancomycin-sensitive strains), Staphylococcus epidermidis (including methicillin-resistant strains), Staphylococcus haemolyticus, Streptococcus spp. viridans:
Gram-negative aerobes: Pasteurella multocida;
gram-positive anaerobes: Clostridium perfringens, Peptostreptococcus anaerobius, Peptostreptococcus spp.
Linezolid-resistant microorganisms:
Haemophilus influenzae, Moraxella catarrhalis, Neisseria spp, Enlerohacteriaceae spp, Pseudomonas spp.
Resistance
Cross-resistance between linezolid and aminoglycosides, ?-lactam antibiotics, folic acid antagonists, glycopeptides, lincosamides, quinolones, rifamycins, streptomycin, tetracyclines, chloramphenecol was not observed due to the difference of linezolid action mechanism from the action mechanisms of these antibacterial agents. Linezolid is active against pathogenic microorganisms both sensitive and resistant to these drugs.
Resistance to linezolid develops slowly by multistep mutation of 23S ribosomal ribonucleic acid (RNA) and occurs at a frequency of less than 1 x10 (-9) to 1 x10 (-11).
Indications
Treatment of infectious and inflammatory diseases when known or suspected to be caused by linezolid-sensitive aerobic and anaerobic gram-positive microorganisms (including infections accompanied by bacteremia):
– Hospital-acquired pneumonia caused by Staphylococcus aureus (methicillin-sensitive strains only) or Streptococcus pneumoniae (including multiresistant strains), including cases accompanied by bacteremia;
– Hospital pneumonia caused by Staphylococcus aureus (methicillin-sensitive and methicillin-resistant strains) or Streptococcus pneumoniae (including multiresistant strains);
– complicated skin and soft tissue infections, including diabetic foot syndrome infections not accompanied by osteomyelitis, caused by Staphylococcus aureus (methicillin-sensitive and methicillin-resistant strains), Streptococcus pneumoniae or Streptococcus agalactiae;
– infections caused by vancomycin-resistant strains of Enterococcus faecium, including those accompanied by bacteremia.
Contraindications
– Hypersensitivity to linezolid and/or other components of the drug.
– Concomitant use of linezolid with monoamine oxidase inhibitors (MAO) A or B (e.g., phenelzine, isocarboxazide), as well as within 14 days after the end of taking the mentioned drugs.
Linezolid should not be prescribed in the absence of blood pressure monitoring and close patient monitoring:
– patients with uncontrolled arterial hypertension, pheochromocytoma, thyrotoxicosis, carcinoid syndrome, bipolar disorder, schizoaffective disorder, acute state of confusion;
– patients receiving the following drugs: adrenomimetics (e.g. pseudoephedrine, phenylpropanolamine, epinephrine, norepinephrine, dobutamine), dopaminomimetics (e.g. dopamine); serotonin reuptake inhibitors, tricyclic antidepressants, serotonin 5-NT1 receptor agonists (triptans), meperidine or buspirone.
Dosage and administration method
- The drug is intended for intravenous administration. Infusion duration is 30-120 min.
- Do not combine infusion bottles (containers) in series and add other drugs to the solution for infusion. If it is necessary to administer linezolid with other drugs, all drugs should be administered separately in accordance with the recommended doses and routes of administration.
- Linezolid for injection is pharmaceutically incompatible with the following drugs: amphotericin B, chlorpromazine, diazepam, phenytoin, erythromycin, lactobionate, cotrimoxazole (trimethoprim + sulfometaxozole), ceftriaxone.
- Compatible solutions for infusion: 5% dextrose solution for injection, 0.9% sodium chloride solution for injection, Ringer-Locke solution for injection.
- Patients to whom the drug was administered intravenously at the beginning of the therapy can be further switched to any dosage form of the preparation for oral administration, dosage adjustment is not required, bioavailability of linezolid during oral administration is almost 100%.
- Dosing regimen and duration of treatment depend on the causative agent, localization and severity of infection and clinical efficacy.
- Recommended dosing regimen for adults and children 12 years of age and older
- Indications (including infections with bacteremia) Dose and administration times Duration of treatment
- Community-acquired pneumonia caused by Staphylococcus aureus (only methicillin-sensitive strains) or Streptococcus pneumoniae (including multiresistant strains), including cases accompanied by bacteremia 600 mg every 12 hours 10-14 days
- Hospital pneumonia caused by Staphylococcus aureus (methicillin-sensitive and megicillin-resistant strains) or Streptococcus pneumoniae (including multiresistant strains) 600 mg every 12 hours 10-14 days
- Complicated skin and soft tissue infections, including diabetic foot syndrome infections not accompanied by osteomyelitis, caused by Staphylococcus aureus (methicillin-sensitive and megicillin-resistant strains), Streptococcus pneumoniae or Streptococcus agalactiae 600 mg every 12 hours 10-14 days
- Infections caused by vancomycin-resistant strains of Enterococcus faecium, including those accompanied by bacteremia 600 mg every 12 hours 14-28 days
- Recommended dosing regimen for children younger than 12 years of age (including newborns*)
- Indications (including infections accompanied by bacteremia) Dose and administration frequency
- Community-acquired pneumonia caused by Staphylococcus aureus (only methicillin-sensitive strains) or Streptococcus pneumoniae (including multiresistant strains), including cases accompanied by bacteremia 10 mg/kg every 8 hours 10-14 days
- Hospital pneumonia caused by Staphylococcus aureus (methicillin-sensitive and methicillin-resistant strains) or Streptococcus pneumoniae (including multiresistant strains) 10 mg/kg every 8 h 10-14 days
- Complicated skin and soft tissue infections, including diabetic foot syndrome infections not accompanied by osteomyelitis, caused by Staphylococcus aureus (methicillin-sensitive and methicillin-resistant strains), Streptococcus pneumoniae or Streptococcus agalactiae 10 mg/kg every 8 h 10-14 days
- Infections caused by vancomycin-resistant strains of Enterococcus faecium, including those accompanied by bacteremia 10 mg/kg every 8 h 14-28 days
- *In preterm infants less than 7 days old (gestation less than 34 weeks), systemic clearance of linezolid is lower and AUC higher than in most neonates and children. By day 7 after birth, linezolid clearance and AUC in preterm infants are close to those of preterm infants and children.
- No dose adjustment is required in elderly patients.
- No dose adjustment is required in patients with renal impairment. Due to the fact that 30% of linezolid is eliminated in hemodialysis within 3 hours, Selezolid should be administered after hemodialysis.
- No dose adjustment is required in patients with hepatic impairment.