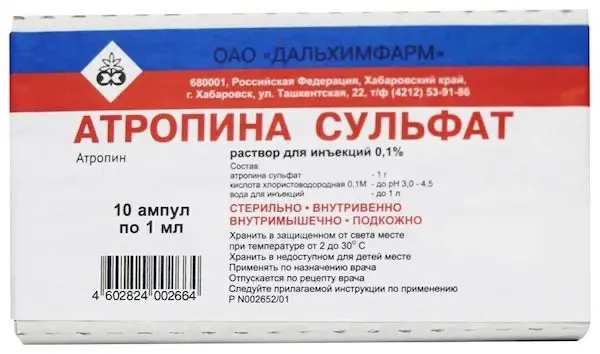
Description
Atropine Sulfate Pharmacodynamics
The alkaloid contained in plants of the family Laspene, M-cholinoreceptor blocker, binds equally to m1-, m2- and mZ-subtypes of muscarinic receptors. It affects both central and peripheral M-cholinoreceptors. It also acts (although much weaker) on n-cholinoreceptors. Prevents the stimulating effect of acetylcholine; reduces the secretion of salivary, gastric, bronchial, lacrimal, sweat glands, pancreas. Reduces muscle tone of internal organs (bronchi, GI organs, bile ducts and gallbladder, urethra, bladder); causes tachycardia, improves atrioventricular (AV) conduction. Reduces gastrointestinal motility, has almost no effect on bile secretion. Dilates pupils, makes it difficult to opacinate intraocular fluid, increases intraocular pressure, causes accommodation paralysis. In medium therapeutic doses has stimulating effect on CNS and delayed but long sedative effect; it excites breathing (high doses – respiratory paralysis). Central anticholinergic effect explains the ability of atropine to eliminate tremor in Parkinson’s disease. Excites cerebral cortex (in high doses), in toxic doses it causes agitation, agitation, hallucinations, coma. It reduces vagus nerve tone, which leads to increased HR (with a slight change in BP) and a slight increase in conduction in the Gis bundle. The effect is stronger with initially increased vagus nerve tone.
After intravenous administration the maximal effect is seen in 2-4 min, after oral administration (as drops) – in 30 min.
Indications
– Gastrointestinal smooth muscle spasm (pylorospasm, intestinal spasms, gallbladder and bile ducts);
– Spasms of the urinary tract;
– gastric and duodenal ulcer (in the acute phase), acute pancreatitis, hypersalivation (parkinsonism, poisoning with salts of heavy metals, dental interventions)
– renal colic;
-hepatic colic;
– bronchospasm, laryngospasm (prevention);
– premedication before surgery;
-Atrioventricular block, bradycardia: poisoning with m-cholinomimetics and anticholinesterase agents.
Contraindications
Hypersensitivity, closed-angle glaucoma or predisposition to it (mydriatic effect leading to increased intraocular pressure may cause an acute attack), tachyarrhythmias, severe chronic congestive heart failure, coronary heart disease, mitral stenosis, reflux esophagitis, esophageal hiatal hernia, pylorus stenosis, hepatic and/or renal failure, bowel atony, myasthenia gravis, urinary retention or its predisposition, diseases accompanied by urinary tract obstruction (incl. including bladder neck due to prostatic hypertrophy), obstructive bowel disease, paralytic ileus, toxic megacolon, nonspecific ulcerative colitis, xerostomia, toxemia of pregnancy, Down’s disease, cerebral palsy, lactation.
Hyperthermia, open-angle glaucoma, chronic heart failure, arterial hypertension, chronic lung diseases, acute blood loss, hyperthyroidism, age older than 40 years (danger of undiagnosed glaucoma), pregnancy.
Pregnancy and lactation:
Atropine penetrates the placental barrier. Adequate and strictly controlled clinical safety studies of atropine use during pregnancy have not been conducted.
Intravenous administration during pregnancy or shortly before delivery may cause fetal tachycardia.
It is not prescribed during pregnancy complicated with gestosis, as it may lead to an increase in blood pressure.
The drug should be used in pregnancy only when the potential benefit justifies the potential risk to the fetus.
Atropine is detected in breast milk in trace concentrations. If it is necessary to use the drug during lactation, breastfeeding should be discontinued.
The drug is contraindicated during breast-feeding.
Directions for use and dosages
- For relieving acute pain of gastric and 12 duodenal ulcer, pancreatitis, renal, hepatic colic, etc., the drug is administered subcutaneously or intramuscularly in 0.25-1 mg (0.25-1 ml of the solution).
- To eliminate bradycardia, the drug is administered intravenously by 0.5-1 mg; if necessary, it may be repeated after 5 minutes.
- For premedication the drug is administered intramuscularly 0.4-0.6 mg 45-60 min before anesthesia.
- In children, the drug is administered at a dose of 0.01 mg/kg.
- In cases of poisoning with m-cholinostimulants and anticholinesterase agents, 1.4 ml of 1 mg/ml solution is administered intravenously, preferably in combination with cholinesterase reactivators.